Definition of Gut
The gut, also known as the gastrointestinal tract or digestive tract, refers to the organs and structures involved in the process of digestion and absorption of nutrients in the body. It starts at the mouth and includes the esophagus, stomach, small intestine, large intestine (colon), rectum, and anus. Continue reading our article to know how to reduce inflammation in the gut.
Gut health refers to the overall well-being and optimal functioning of the gastrointestinal (GI) tract, which includes the stomach and other organs involved in digestion It involves maintaining a balance of beneficial bacteria, proper digestion and absorption of nutrients, effective immune responses, and smooth elimination of waste. Taking steps to prioritize and improve gut health can support leaders in maintaining optimal health, vitality, and performance in their professional roles.

According to Gerard Mullin, M.D., a gastroenterologist at Johns Hopkins, “As we get older, the natural processes slow down and become less efficient.” Taking care of your gut health can involve adopting a balanced and nutritious diet, staying hydrated, managing stress, getting regular exercise, and avoiding behaviors that can disrupt the gut microbiota, such as excessive alcohol consumption or overuse of antibiotics.
Understanding the Causes of Gut Disruptions
- Frequent travel or dining out for business purposes can present challenges in maintaining a healthy gut. Limited food options, exposure to unfamiliar cuisines, and disrupted routines can impact digestive health.
- People often prioritize work over self-care, which can lead to neglecting healthy habits like exercise, relaxation, and adequate sleep. These factors are crucial for maintaining a healthy gut.
- Erratic schedules and long work hours can lead to irregular meal patterns, including skipping meals or eating on the go. This can disrupt digestion and negatively impact gut health.
- The gut-brain axis serves as a vital communication pathway, an intricately gut-brain connection. This can impact the ability to manage stress, make sound judgments, and maintain positive relationships with team members.
- The gut plays a crucial role in immune function. A compromised gut can lead to a weakened immune system, making individuals more susceptible to infections, frequent illnesses, and longer recovery times.
- Excessive alcohol consumption contributes to digestive problems and disturbs the equilibrium of beneficial gut bacteria, resulting in changes to the composition of the gut microbiota.
- Overuse of antibiotics can disturb the balance of the gut microbiota, leading to a condition called dysbiosis. Dysbiosis can result in digestive problems such as diarrhea, bloating, and abdominal discomfort.
Digestive Disorders Associated with Organs
Please note that these are just a few examples, and there are several other digestive disorders that exist. Here are the common digestive disorders:
- Gastroesophageal Reflux Disease (GERD)
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease (IBD) (includes Crohn’s disease and ulcerative colitis)
- Peptic Ulcer Disease
- Celiac Disease
- Gallstones
What is the Microbiome?
The microbes and other bacteria in your gut help you digest food and may support heart, brain health, immune system, and overall well-being. The microbiome refers to the community of microorganisms, including bacteria, viruses, fungi, and other microbes, that reside in and on the human body. The human gut microbiome consists of approximately 200 different species. The gut microbiome specifically refers to the microorganisms present in the gastrointestinal tract.
While certain microorganisms can be detrimental to our health, numerous others are highly beneficial and crucial for maintaining a healthy body. Extensive research suggests that a diverse range of bacteria in the gut can potentially lower the risk of various conditions, including diabetes, inflammatory bowel disease, and psoriatic arthritis.
Understanding the Role of Gut Microbiome
- The gut microbiome aids in the digestion of dietary fibers, complex carbohydrates, and other substances that our body cannot break down on its own.
- It helps educate immune cells, ensuring they respond appropriately to pathogens while maintaining tolerance to harmless substances.
- The gut microbiome contributes to maintaining the integrity of the gut barrier, which is crucial for preventing the entry of harmful substances into the bloodstream.
- Certain microbes in the gut microbiome produce essential compounds, such as vitamins (e.g., vitamin K, some B vitamins) and short-chain fatty acids (SCFAs).
- The gut microbiome produces neurotransmitters, such as serotonin and dopamine, which impact mood and cognition.
- A healthy gut microbiome is associated with a reduced risk of various conditions, including gastrointestinal disorders (e.g., irritable bowel syndrome, inflammatory bowel disease), metabolic disorders (e.g., obesity, type 2 diabetes), cardiovascular diseases, and even certain cancers.
A Naturopathic Perspective to enhance gut health
Dr. Kaylee uses a naturopathic approach to improve gut health which involves supporting liver function. As the liver plays a crucial role in making bile acid, which helps keep bacteria in check, and stimulates peristalsis. Supporting liver health can indirectly benefit gut health by optimizing the elimination of toxins and waste products from the body. Naturopathic practitioners may utilize herbal remedies to support the function of the liver and the gut. They also suggest a gut-brain connection diet.
How to reduce inflammation in the gut?
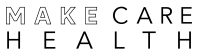
The gut-brain connection diet refers to an eating approach that focuses on promoting a healthy gut microbiome and supporting optimal brain function. It includes a variety of fiber-rich foods such as fruits, vegetables, whole grains, legumes, and nuts. This diet also helps to reduce inflammation in the gut.
Herbs such as aloe vera, chamomile, peppermint, ginger, and licorice root have been traditionally used to soothe digestive discomfort, reduce inflammation, and promote healthy digestion.
Naturopathic practitioners suggest specific nutrients and supplements that support gut healing, such as omega-3 fatty acids, glutamine, zinc, and vitamins A, C, and E. These nutrients can help reduce inflammation, support gut lining integrity, and promote healthy immune function. Probiotic supplements may also be recommended based on individual needs and conditions.
Pro tip: It’s important to note that the gut-brain connection diet is not a one-size-fits-all approach, and individual needs may vary.
Tracking Digestive Health By Essential Biomarkers to Monitor
Unveiling Digestive Efficiency: The Power of Transit Time or the Beet Test
- Consume one large or a few medium-sized beets (raw or cooked) in the evening if you haven’t had them for about a week.
- Make a note of the last time you observe a red tint in your stool (urine color is not a concern).
- Repeat the test a few times, with a few days’ break between each beet consumption, to establish an average.
- This method aids in determining the duration it takes for food to pass through your gastrointestinal (GI) tract.
Exploring the Profound Meaning Behind Your Bowel Movements
- Observe your stool: Is it well-formed, watery, soft, sticky, or breaking apart? Noting these details assists your naturopathic doctor in assessing your condition.
- Utilize the Bristol Stool chart as a reference to determine the consistency and form of your stool.
- Additionally, keep track of any factors that may influence your stool, such as mood, diet, stressors, or lifestyle habits. This information aids in comprehending the impact of these factors on your stool outcomes.
Understand Your Digestive Rhythm by Monitoring Bowel Regularity
- Aim for an ideal frequency of 1-3 bowel movements per day.
- Take note of any variations in frequency, especially if you experience episodes of diarrhea or loose stools.
- If you tend towards constipation with infrequent bowel movements (e.g., every other day or longer), maintain a journal to accurately track the frequency, ease of passage, and form of your stools.
- Consider how your mood, emotions, food choices, stress levels, and lifestyle factors may influence your bowel movements.
- These practices serve as valuable data points for evaluating your gut health biomarker, known as transit time.
- You can try implementing these monitoring techniques under the guidance of a naturopathic doctor as part of our Digest Your Best – Gut Treatment Program.
How coffee destroys gut flora?
No coffee does not destroy gut flora. It does not have a detrimental effect on gut bacteria. Research indicates that both regular and decaffeinated roasted coffee can support the growth of probiotic strains due to their prebiotic properties.
Moreover, individuals who regularly consume coffee have been observed to possess higher levels of anti-inflammatory bacteria like Faecalibacterium and Roseburia, while having lower levels of pathogens such as Erysipelatoclostridium, in comparison to non-coffee drinkers. Kerry Beeson, BSc (Nut. Med.), a qualified nutritional therapist, also supports the idea.
How do probiotics affect the gut flora?
Probiotics, as beneficial microorganisms, have the ability to regulate the balance of intestinal flora and boost immunity. They enhance the immune system by preserving the integrity of the epithelial barrier, preventing pathogens from attaching to the intestinal surface and modulating and promoting the proper development of the immune system.
Coffee, being a daily consumption habit for many adults, provides an excellent foundation for incorporating probiotics that require daily supplementation, explains Liu Shao Quan, MS, Ph.D ., a food science professor at the National University of Singapore who led the research, tells Verywell. “By infusing probiotics into a commonly consumed beverage, we can make the benefits of probiotics more readily available to a broader and mainstream audience.”
Most types of probiotic bacteria are sensitive to heat and can be killed by it. Therefore, it is not recommended to mix probiotics into hot drinks. However, once your tea or coffee has cooled down to a temperature closer to the body’s warmth, probiotics can withstand it. So, the straightforward answer is no, you don’t need to be concerned about taking probiotics while enjoying your morning coffee. Ideally, it is suggested to swallow your probiotic supplement with a sip of water, in between sips of your delightful hot beverage.
Taking probiotics with hot drinks – a checklist
- Mixing a probiotic sachet/capsule with a hot drink (e.g., coffee): Bad idea!
- Swallowing probiotic capsules with a hot drink: Probably fine, but not ideal.
- Taking probiotics with a cold drink (preferably milk or water), in between sips of a hot drink: Yes, this is perfect!
- Taking probiotics with cold milk or water, then waiting 30 minutes before having a hot drink: Fine, but not necessary.